Informacje o artykule
DOI: https://www.doi.org/10.15219/em104.1652
W wersji drukowanej czasopisma artykuł znajduje się na s. 23-33.
 Pobierz artykuł w wersji PDF
Pobierz artykuł w wersji PDF
 Abstract in English
Abstract in English
Jak cytować
Bąk, D., & Bąk, S. (2024). Change management in healthcare - a scoping literature review. e-mentor, 2(104), 23-33. https://doi.org/10.15219/em104.1652
E-mentor nr 2 (104) / 2024
Spis treści artykułu
Informacje o autorach
Change management in healthcare - a scoping literature review
Danuta Bąk, Sylwia Bąk
Abstract
The healthcare sector is constantly changing due to many different factors, both external and internal, such as regulatory, organizational, technological, personnel, financial, and geopolitical change. Change management methods and tools are useful for effectively planning, implementing and monitoring change. The important issue is in which areas and to what extent change management is utilized in healthcare. The aim of this text is therefore to conduct a scoping literature review on change management in healthcare and to develop, based on the results of this research, a theoretical model of determinants and motives for implementing change management in healthcare. A scoping review of the literature was conducted to determine the extent to which change management is applied in healthcare organizations. Texts meeting the inclusion criteria were searched for in four databases: PubMed, Embase, Scopus, and EBSCO. The search was limited to texts published in English. Of the 247 publications screened, 73 met the inclusion criteria. Additionally, 1021 keywords were selected from the screened publications, of which 137 met the inclusion criteria and were approved for the keyword analysis. The keywords formed seven thematic clusters: human, change management, organization and management, leadership, healthcare delivery, hospital management, and productivity. There are a number of motives for using change management in healthcare, and all centre around a few determinants that can be divided into those directly related to the specifics of the healthcare sector and those directly related to management processes. These determinants and motives were included in the theoretical model.
Keywords: change management, healthcare, hospital, medicine, scoping review
Introduction
The healthcare sector is one of the most important sectors of the global economy, and indispensable for its stable functioning (Boyce & Brown, 2019). Today, its role is even more accentuated, particularly due to the past COVID-19 pandemic, which caused a number of diverse problems for entities in this sector (Jedynak & Bąk, 2021). For several decades, in times of systemic changes, crises, and reforms of the healthcare sector, changes have been introduced in various regions of the world to increase the quality of health services provided, improve access to them, introduce upgrades and innovations in line with technological advances, and improve the efficiency of the operational tasks carried out by healthcare organizations (Deloitte Global, 2022).
To make these changes more effective, advanced management methods and tools need to be implemented in the healthcare sector (Bąk, 2022). What attracts considerable attention due to its effectiveness in this as well as other sectors, is the methods and tools of change management, which enable professional management of planning, implementing, and monitoring operational, strategic, and systemic changes in healthcare organizations (Harrison et al., 2021).
The results of many scientific studies (e.g. Al-Abri, 2007; Igoe, 2021; Yousefi et al., 2022) indicate that change management is vital in the healthcare sector, particularly in times of turbulence and crisis. However, change management methodologies are not yet widely used in reforming the healthcare sector globally. In contrast, where professional change management in healthcare organizations is used, it has proven to be very effective and has been welcomed by healthcare managers and executives as well as employees and patients (Nilsen et al., 2020).
In order for healthcare organizations to better understand and take advantage of change management methods and tools, identification and diagnostic studies in this area are needed. This scoping review aims primarily to identify areas of healthcare where changes, improvements, and enhancements are implemented using management methods based on change management.
Methods
The main aim of the research was to identify existing research evidence regarding change management in healthcare. With respect to the research area under consideration, an approach to the analysis of the literature in terms of its existing scope seems most reasonable. To achieve the main research aim, two specific aims were set:
- to conduct a scoping literature review on change management in healthcare,
- to develop a theoretical model of determinants and motives for implementing change management in healthcare.
The main method used in the research procedure was therefore a scoping review of the literature on the subject (Armstrong et al., 2011; Munn et al., 2018). Consequently, the authors followed the methodological rigour of this research method (Arksey & O'Malley, 2005; Levac et al., 2010; Peters et al., 2015). Furthermore, during the final analysis of the substantive content of the texts, the authors used the method of logical categorization, satisfying the criteria of exhaustiveness and separability required by the rigour of this method when creating categories (Bailey, 1994; Saran, 2014):
— exhaustiveness:
- all keywords were included in a substantively adequate cluster (Table 1),
- all texts were included in a substantively adequate category of scope (Table 3).
— separability:
- each keyword is allocated to only one cluster (Table 1),
- each text is allocated to only one category of scope (Table 3).
In order to develop a theoretical model of determinants and motives for implementing change management in healthcare, an exploratory approach to research was adopted (Saunders et al., 2009). Using this research approach, the determinants of change management in healthcare were defined based on clusters of keywords of the analysed texts identified in the research process. Moreover, based on the categories of scope of the analysed texts identified in the research process, the motives for implementing change management methods and tools in healthcare were defined. Then, the authors determined the relationships and activities connecting the defined determinants and motives, and thus an original theoretical model of change management in healthcare was created.
Search strategy
The authors searched for the literature on the subject in four databases: PubMed, Embase, Scopus, and EBSCO. The choice of databases was not random. In view of the fact that the research area under consideration is multidisciplinary and is a point of intersection between healthcare and management, the authors selected two medical databases and two multidisciplinary databases in order to increase the probability of finding most of the scientific texts on the topic of change management in healthcare published to date. The authors applied the following initial search criteria: 1) articles and peer-reviewed conference proceedings in English only, 2) the occurrence of established headwords at the level of text titles. The authors compiled a list of 36 headwords representing exhaustive possibilities for identifying the topics of articles the authors were interested in. On this basis, the authors established search queries tailored to the search systems in the respective databases. The overall strategy adopted for searching texts in the databases is shown in Figure 1.
Figure 1
Search strategy
Source: authors' own work.
Article selection
The final number of texts to be examined was selected in two steps (Step I and Step II).
Step I - in the first step, the texts retrieved from the databases, based on the strategy presented in Figure 1, were purged of duplicate items.
Step II - in the second step, from the list of publications created in Step I, the authors selected only those available in Open Access. Then, from the remaining texts available as the full text, the authors eliminated texts with specific subject matters not directly relevant to the research issue under consideration.
Data extraction and analysis
The authors continued the process of data extraction and analysis, using also a two-step scheme (Step I and Step II).
Step I - in the first step, the texts approved at the article selection stage underwent a quantitative and qualitative keyword analysis based on the VOSviewer software. The qualitative analysis concerned the substantive assessment and the meaning of keywords, while the quantitative analysis concerned the frequency and repetition of individual keywords and subtraction of those keywords that did not pass the substantive assessment: the set of the keywords gathered from all the texts was cleared of those that were not relevant to the research objectives. The remaining keywords were grouped into thematic clusters adequately reflecting the scope of the research topic under analysis. The authors presented these clusters according to frequency of occurrence in the texts and the network of relationships among the keywords, as well as in chronological order.
Step II - in the second step, the authors analysed the texts approved at the article selection stage in terms of their substantive content. For this purpose, the authors performed a logical categorization.
The study selection process is presented in detail in Figure 2.
Figure 2
Flow chart showing the text selection process
Source: authors' own work.
Results
Search results
The results of the search and application of the defined inclusion and exclusion criteria of the retrieved texts were consistently divided into Step I and Step II, according to the established research procedure (Figure 2).
Step I - in the first step, using a keyword search strategy (Figure 1), the authors retrieved from the databases a total of 505 publications with at least a title, abstract, and keywords available. The number of the publications obtained from the respective databases was as follows: PubMed (118), Embase (151), Scopus (202), and EBSCO (34). The database search process was carried out in June 2023. After eliminating duplicate items (258), the authors were left with a publication list of 247 items meeting the inclusion criteria indicated above (Figure 2).
Step II - in the second step, from the list of the publications accepted in Step I, the authors deleted all texts that were not available as the full text (161). Thus, the authors identified 86 publications available in Open Access for further analysis. The authors then analysed the texts' titles and abstracts with regard to their substantive content and excluded those that were of a specific nature, not directly related to the issue of change management in healthcare. These were, for example, texts on veterinary medicine or bio-medical ontologies. On this basis, the authors eliminated thirteen texts from the list and, consequently, approved 73 texts for the final analyses.
Scope
The analysis of the scope of the collected publications was also performed in two steps (Step I and Step II). The scope was determined based on a quantitative-qualitative analysis.
Step I - the search for keywords in all 247 publications produced a total of 1021 items. The authors then filtered out the keywords that were repeated in three or more texts, considering their repetition as a criterion of representativeness. On this basis, the collected list of keywords was reduced to 163 items approved for further analyses. Following individual selection after excluding keywords with no substantive connection to the subject matter under examination, such as country names, article, review, etc. (26), the authors eventually included 137 keywords in the scope analysis. These were categorized in the VOSviewer software and divided into seven thematic clusters. Each cluster showed network links and relationships between the keywords contained within it. Altogether, the authors identified 1879 links and 3501 total link strength. At the centre of each cluster were the following keywords:
Cluster 1 - human (occurred in 103 texts),
Cluster 2 - change management (occurred in 91 texts),
Cluster 3 - organization and management (occurred in 61 texts),
Cluster 4 - leadership (occurred in 32 texts),
Cluster 5 - healthcare delivery (occurred in 21 texts),
Cluster 6 - hospital management (occurred in 14 texts),
Cluster 7 - productivity (occurred in four texts).
The keyword clusters are presented in Table 1.
Table 1
Keyword clusters
Total link strength |
Occurrences |
Keyword |
Cluster |
Keyword |
Occurrences |
Total link strength |
| 48 | 5 | Clinical practice | 5 | Community care | 8 | 60 |
| 71 | 7 | Consultation | 5 | Controlled study | 5 | 43 |
| 32 | 4 | Cooperation | 5 | Decision making | 5 | 29 |
| 21 | 4 | Economic aspect | 5 | Decision making | 4 | 28 |
| 57 | 5 | Financial management | 5 | General practitioner | 3 | 28 |
| 22 | 3 | Government | 5 | Healthcare delivery | 21 | 148 |
| 101 | 14 | Healthcare management | 5 | Healthcare organization | 14 | 98 |
| 106 | 13 | Healthcare quality | 5 | Healthcare system | 8 | 68 |
| 34 | 3 | Health program | 5 | Health promotion | 3 | 10 |
| 148 | 19 | Health service | 5 | Health services research | 6 | 55 |
| 34 | 3 | Hospital care | 5 | Medical care | 7 | 13 |
| 89 | 13 | Medical education | 5 | Medical profession | 4 | 41 |
| 89 | 13 | Medical education | 5 | Medical profession | 4 | 41 |
| 33 | 4 | Medical school | 5 | Medical staff | 3 | 29 |
| 52 | 6 | Medical student | 5 | Mental health | 3 | 21 |
| 100 | 10 | Patient care | 5 | Pharmacist | 3 | 18 |
| 38 | 4 | Physician attitude | 5 | Primary Healthcare | 5 | 31 |
| 44 | 6 | Public health | 5 | Public hospital | 4 | 25 |
| 41 | 3 | Society | 5 | Teaching | 4 | 46 |
| 39 | 4 | Work environment | 5 | |||
| 23 | 3 | Adaptive behaviour | 3 | Administrative personnel | 3 | 24 |
| 44 | 4 | Behaviour | 3 | Evaluation study | 4 | 40 |
| Healthcare facility | 3 | Healthcare planning | 8 | 77 | ||
| 110 | 15 | Healthcare policy | 3 | Hospital organization | 10 | 74 |
| 17 | 4 | Hospital subdivisions and components | 3 | Information system | 3 | 15 |
| 77 | 8 | Interpersonal communication | 3 | Medical informatics | 7 | 36 |
| 35 | 4 | National health service | 3 | Nurse administrator | 4 | 43 |
| 439 | 55 | Organization | 3 | Organization and management | 61 | 495 |
| 36 | 5 | Personnel management | 3 | Professional standard | 4 | 40 |
| 46 | 5 | Public relations | 3 | Social change | 4 | 29 |
| 49 | 6 | Standard | 3 | Workforce | 5 | 51 |
| 48 | 3 | Cost | 6 | Database | 3 | 52 |
| 22 | 3 | Delivery of Healthcare | 6 | Documentation | 3 | 55 |
| 89 | 8 | Economics | 6 | Health facilities | 14 | 113 |
| 81 | 6 | Health personnel attitude | 6 | Hospital cost | 3 | 53 |
| 97 | 8 | Hospital department | 6 | Hospital information system | 4 | 64 |
| 123 | 14 | Hospital management | 6 | Humans | 7 | 66 |
| 59 | 5 | Mass communication | 6 | Medical record | 5 | 62 |
| 94 | 7 | Nursing stuff | 6 | Operating room | 5 | 42 |
| 57 | 4 | Organizational innovation | 6 | Practice guideline | 5 | 61 |
| 82 | 6 | Psychological aspect | 6 | Software | 5 | 42 |
| 120 | 11 | University hospital | 6 | |||
| 27 | 3 | Case report | 1 | Change | 3 | 10 |
| 38 | 4 | Coronavirus disease 2019 | 1 | Emergency care | 5 | 50 |
| 46 | 4 | Follow up | 1 | General hospital | 3 | 24 |
| 21 | 3 | Healthcare cost | 1 | Human | 103 | 795 |
| 44 | 7 | Human experiment | 1 | Information processing | 9 | 84 |
| 23 | 3 | Organizational culture | 1 | Pandemic | 5 | 38 |
| 46 | 6 | Procedures | 1 | Program development | 3 | 23 |
| 55 | 8 | Qualitative research | 1 | Quality control | 4 | 30 |
| 30 | 3 | Retrospective study | 1 | Skill | 4 | 37 |
| 13 | 3 | Strategic planning | 1 | University | 3 | 31 |
| 28 | 3 | Vision | 1 | |||
| 28 | 3 | Adoption | 4 | Check list | 4 | 37 |
| 39 | 3 | Clinical audit | 4 | College | 3 | 32 |
| 110 | 11 | Education | 4 | Electronic medical record | 5 | 55 |
| 31 | 3 | Funding | 4 | Healthcare personnel | 8 | 54 |
| 143 | 16 | Hospital | 4 | Hospital administrator | 4 | 23 |
| 302 | 32 | Leadership | 4 | Manager | 7 | 75 |
| 92 | 8 | Nurse | 4 | Physician | 11 | 121 |
| 33 | 3 | Planning | 4 | Risk | 3 | 33 |
| 38 | 5 | Teaching hospital | 4 | Telehealth | 3 | 13 | 472 | 91 | Change management | 2 | Change management process | 3 | 14 |
| 31 | 7 | Health | 2 | Healthcare | 16 | 93 |
| 9 | 3 | Healthcare system | 2 | Healthcare | 5 | 10 |
| 9 | 4 | Hospitals | 2 | Implementation | 3 | 9 |
| 9 | 3 | Implementation science | 2 | Information systems | 5 | 26 |
| 32 | 6 | Information technology | 2 | Information use | 4 | 19 |
| 91 | 15 | Management | 2 | Organizational change | 5 | 6 |
| 83 | 9 | Total quality management | 2 | |||
| 31 | 4 | Job satisfaction | 7 | Organizational structure | 3 | 20 |
| 45 | 4 | Productivity | 7 |
Source: authors' own work.
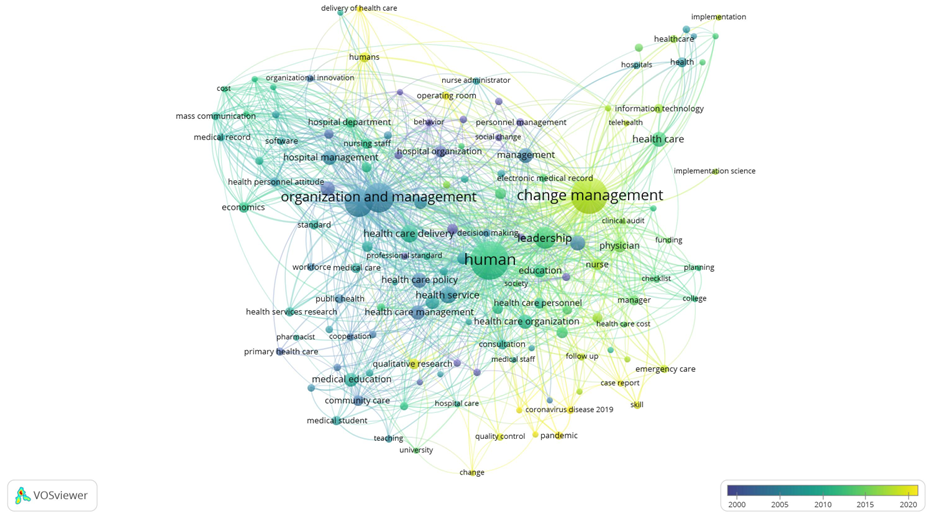
The network of links in the thematic clusters of the keywords is presented in Figure 3.
Figure 3
Network of links among the keywords
Source: authors' own work.
In determining the scope of the literature on the area under analysis, it is extremely important to arrange the thematic content appearing in the selected texts chronologically. The 247 texts selected and included in the analyses in Step I had publication dates beginning in 1969 and ending in 2023, which confirmed the continuous development of the issues in scientific literature. The chronological changes in the emerging keywords are shown in Figure 4.
Figure 4
Chronological distribution of the keywords
Source: authors' own work.
Table 2 shows the chronological distribution of the texts approved for the keyword analysis in Step I, divided into single-author and multi-author texts.
Table 2
Chronological distribution of the selected texts
Time span |
Number of publications |
Single-author texts |
Multi-author texts |
| 1969-1979 | 7 (3%) | 6 (86%) | 1 (14%) |
| 1980-1990 | 17 (7%) | 13 (76%) | 4 (24%) |
| 1991-2001 | 31 (13%) | 23 (74%) | 8 (26%) |
| 2002-2012 | 75 (30%) | 31 (41%) | 44 (59%) |
| 2013-2023 | 117 (47%) | 29 (25%) | 88 (75%) |
Source: authors' own work.
Step II - After obtaining the final number of texts approved for the final analyses (73), the authors categorized them by scope, creating factual categories of healthcare areas in which change management was evidently applied. This scope categorization is presented in Table 3.
Table 3
Scope categorization
| Category | Publications (in chronological order) |
Number of publications | ||
| number | % | |||
| Digital transformation and innovations | Shaban-Nejad & Haarslev (2007); Hutchinson (2023); Shoolin (2010); Swecker et al. (2010); Kulhanek (2011); Takian (2012); Grandpierre et al. (2016); ChePa et al. (2017); ChePa et al. (2018); Ileri & Arik (2018); Ningtyas et al. (2020); Threatt et al. (2020); Hospodková et al. (2021); Razmak et al. (2021); Ferrara et al. (2022); Martens et al. (2022); Yusif et al. (2022) | 17 | 23 | |
| Fundamental management processes and employees | Al-Abri (2007); Allen & Stevens (2007); Mazur et al. (2010); Lee et al. (2011); Macphee & Suryaprakash (2012); Shipton et al. (2014); Gibbons et al. (2021); Harrison et al. (2022); Turja (2022); Pachamanova et al. (2022); Yousefi et al. (2022); Harris (2023); Webster (2023) | 13 | 18 | |
| Education | Godbolt et al. (1997); Thistlethwaite (2000); Agius et al. (2008); Chandran et al. (2013); Enăchescu & Trapiel (2014); Al-Moosa & Sharts-Hopko (2017); Barker et al. (2020); Ward et al. (2020); Vickers et al. (2021); Karimi et al. (2022); Li et al. (2022); Torkzadeh & Mohtaram (2022) | 12 | 16 | |
Medical specialization modules |
Cardiology | Alsunbuli (2020) | 11 | 15 |
| Pharmacology | Deavin et al. (2023) | |||
| Oncology | Divaris & Srigley (2012); Sale et al. (2019) | |||
| Surgery | Neuwirth et al. (2021); Farrelly (2022) | |||
| Neurology | Karlsson & Nordström (2022) | |||
| Psychiatry | Kingsley (1993); Ritson & Waterfield (2005) | |||
| Pediatrics | Law et al. (2011) | |||
| Gynecology | Sobkowski & Opala (2014) | |||
| Implementation of professional management methods | Soft Systems Methodology | Augustsson et al. (2019a; 2019b) | 5 | 7 |
| Lean Healthcare | Maravi-Cardenas et al. (2020); van Rossum et al. (2016) | |||
| Action research | Margulies (1977) | |||
| Disparities in healthcare | Coombe (2008); Pratt et al. (2012); Odaga et al. (2016); Betancourt et al. (2017); Carman et al. (2019) | 5 | 7 | |
| Reforming of healthcare | Casebeer et al. (2000); Villalbí & Farrés (2005); Kiernan & Tunney (2016); Javanparast et al. (2018) | 4 | 6 | |
| Financing of healthcare | Carlson (2009); Ruhl & Klöss (2012); Walsh (2016) | 3 | 4 | |
| Standardization | Appleby & Tempest (2006); Bourke et al. (2016); Harrison et al. (2021) | 3 | 4 | |
Source: authors' own work.
The analyses determined that the substantive areas of the texts approved for the analyses formed coherent categories, adequately reflecting the areas of healthcare change management methods and tools were applied effectively. A majority of the analysed texts (23%) concerned change management in healthcare in the areas of digital transformation and implementation of innovations. The authors observed an intensification of this trend from 2020, i.e. the year of the COVID-19 pandemic, during which digitalization, innovation, and the development of telemedicine became some of the most important areas of change in healthcare. The second area in which change management was applied in the healthcare sector was fundamental management processes in the management of healthcare facilities, mainly related to changes in procedures concerning individual groups of employees. Medical education and medical specialization modules constitute two further healthcare areas undergoing intensive change implementation processes. The subsequent categories relate to the use of change management tools for: 1) implementing professional management methods (e.g. Lean Management or Action Research) in healthcare, 2) addressing disparities in healthcare, 3) reforming the healthcare system, 4) healthcare financing, and 5) standardizing procedures in healthcare.
Discussion
The most frequently adapted change management models in healthcare include Lewin's 3-Stage Model (Mind Tools, n.d.) and Kotter's 8-Step Model (Kotter, 1995). These models have an application and practical dimension, which means that in many cases they are used to implement change management tools in specific dimensions of the functioning of healthcare units, e.g. optimizing the work of doctors and nurses, improving the efficiency of operating theaters and hospital wards, improving the quality of patient care, etc. These models are currently successfully implemented in various projects to improve healthcare units (Harrison et al., 2021).
The model that includes the determinants and motives of change management in healthcare, which was developed by the authors of this text (Figure 5), differs from the practical models discussed above, because it has a theoretical dimension. It is the result of modelling the scope of use of change management tools in healthcare. It does not cover the analysed topic fragmentarily, but holistically, and indicates paths for the possible use of change management in the examined sector. It is therefore the basis for designing application solutions that can be implemented in healthcare units. Therefore, this model can be considered the first step in planning modern solutions that improve how the sector functions based on professional change management methods and tools.
Modelling the scope of change management in healthcare
The articles analysed in the review presented in this paper made it possible to determine clearly the scope of the texts in the thematic area of change management in healthcare. By categorizing their topics and analysing their keywords, it is possible to model not only the scope of the scientific literature on this topic, but also the main motives for using professional change management methods to improve and develop the healthcare sector. The authors therefore undertook to create a model reflecting the main determinants of and motives for change management in healthcare (Figure 5).
Figure 5
Determinants of and motives for change management in healthcare - a theoretical model
Source: authors' own work.
The main determinants of change management in healthcare can be divided into those directly related to the specifics of the sector and those directly related to management processes. Sector-specific determinants include patients, delivery of healthcare, and management of healthcare entities, while those directly related to management include organization of management processes, system productivity, and leadership.
The analysis identified the following the motives for implementing change management in healthcare:
- reforming the entire healthcare system in order to correct inadequacies in the delivery of healthcare services, as well as improving the management procedures in healthcare entities,
- implementing digital transformation and innovations across the healthcare sector with a view to extending the scope and improving the quality of healthcare services, and modernizing management methods and techniques,
- redressing inequalities in patients' access to health services and eliminating other disproportions in their delivery processes,
- ensuring an adequate range and level of education of medical personnel, which determines the continuity of healthcare delivery and quality improvement,
- developing medical specialization modules in the provision of increasingly sophisticated healthcare services,
- basing the management of healthcare entities on medical specialization modules, which should constitute the core of the functioning of the whole system,
- ensuring access to sources of funding allowing for the continuous development of healthcare entities,
- implementing professional management methods in organizational leadership development,
- applying professional management methods as a standard procedure in the organization and management of healthcare entities,
- performing all basic management processes in the management of healthcare entities with particular focus on the processual nature of the fulfilment of duties by individual groups of employees,
- applying proven standards for the development of management processes,
- utilizing the advantages of standardization in improving the operational and strategic efficiency of healthcare entities.
Limitations
This scoping review has several limitations. Firstly, it comprised searches for texts based on keywords appearing in their titles. Thus, despite a very deliberate strategy to search for texts in as many as four databases, there must have been other texts meeting the inclusion criteria that were not indexed in the selected databases and, consequently, were not included in the review. Another limitation of the conducted research may be the inclusion of only scientific texts published in English in the analyses.
The fact that not all texts were available on an open access basis can be considered a further limitation. The option of reading the full version of a given text in order to gain a precise understanding of its factual content was one of the inclusion criteria for approving selected papers for the final analyses. Thus, a number of texts were not included due to accessibility constraints, and their inclusion in the study could have broadened the scope of the final conclusions.
Conclusions
The conducted research achieved both the main research aim and two intended specific aims. This review succeeded in identifying the scope of the scientific literature on the topic area of change management in healthcare. Furthermore, through keyword analysis and the categorization of the keynotes of the texts included in the analyses, it was possible to create a model indicating the main determinants of and motives for using change management in correcting, developing, and improving the healthcare sector. Thanks to the conducted research, it was possible to fill the research gap regarding the deficit of scientific texts indicating the scope of literature on change management in healthcare and modelling the motives for implementing change management in this sector.
The theoretical framework resulting from the performed analyses can be used by healthcare managers and decision-makers in various practical applications as well as academics and researchers specializing in healthcare management. This is extremely relevant at the present time, when the healthcare sector worldwide is recovering from the pandemic crisis, while simultaneously facing the challenges of digitalization. In addition, problems with access, coverage, and quality of healthcare services in different regions of the world are still evident. Therefore, it is particularly important to develop new research threads regarding correcting and improving management in healthcare units. New methods of change management, risk management, and quality management implemented in healthcare should therefore constitute the directions of future scientific research.
References
- Agius, S., Willis, S., McArdle, P., & O'Neill, P. (2008). Managing change in postgraduate medical education: still unfreezing? Medical Teacher, 30(4), e87-e94. https://doi.org/10.1080/01421590801929976
- Al-Abri, R. (2007). Managing change in healthcare. Oman Medical Journal, 22(3), 9-10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3294155/pdf/OMJ-D-07-00001.pdf
- Allen, C., & Stevens, S. (2007). Health service integration: a case study in change management. Australian Health Review, 31(2), 267-275. https://doi.org/10.1071/AH070267
- Al-Moosa, N. H., & Sharts-Hopko, N. (2017). Using change management to redesign Oman?s Health Professions Education Sector. Health Professions Education, 3(2), 108-112. https://doi.org/10.1016/j.hpe.2016.09.001
- Alsunbuli, A. (2020). Leadership and change management in advancing hybrid operating rooms into interventional cardiology in hospitals within the National Health Service. Future Healthcare Journal, 7(1), s6-s7. https://doi.org/10.7861/fhj.7.1.s6
- Appleby, H., & Tempest, S. (2006). Using change management theory to implement the International Classification of Functioning, Disability and Health (ICF) in clinical practice. British Journal of Occupational Therapy, 69(10), 477-480. https://doi.org/10.1177/030802260606901007
- Arksey, H., & O'Malley, L. (2005) Scoping studies: towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19-32. https://doi.org/10.1080/1364557032000119616
- Armstrong, R., Hall, B. J., Doyle, J., & Waters, E. (2011). 'Scoping the scope' of a cochrane review. Journal of Public Health, 33(1), 147-50. https://doi.org/10.1093/pubmed/fdr015
- Augustsson, H., Churruca, K., & Braithwaite, J. (2019a). Mapping the use of soft systems methodology for change management in healthcare: A scoping review protocol. BMJ Open, 9(4), e026028. https://doi.org/10.1136/bmjopen-2018-026028
- Augustsson, H., Churruca, K., & Braithwaite, J. (2019b). Re-energising the way we manage change in healthcare: the case for soft systems methodology and its application to evidence-based practice. BMC Health Services Research, 19(1), 666. https://doi.org/10.1186/s12913-019-4508-0
- Bailey, K. D. (1994). Typologies and taxonomies. An introduction to classification techniques. SAGE Publications, Inc. https://doi.org/10.4135/9781412986397
- Bąk, D. (2022). Methods and tools of Lean Management in hospital management - case studies. Zdrowie Publiczne i Zarządzanie, 20(2), 34-46. https://doi.org/10.4467/20842627OZ.22.008.17641
- Barker, S., Ali, F., & Tsitsiou, Y. (2020). Students as catalysts for curricular innovation: A change management framework from the medical students perspective. Medical Teacher, 42(12), 1428-1429. https://doi.org/10.1080/0142159X.2020.1739258
- Betancourt, J. R., Tan-McGrory, A., Kenst, K. S., Phan, T. H., & Lopez, L. (2017). Analysis & commentary: Organizational change management for health equity: Perspectives from the disparities leadership program. Health Affairs, 36(6), 1095-1101. https://doi.org/10.1377/hlthaff.2017.0022
- Bourke, A., Bate, A., Sauer, B. C., Brown, J. S., & Hall, G. C. (2016). Evidence generation from healthcare databases: recommendations for managing change. Pharmacoepidemiology and Drug Safety, 25(7), 749-754. https://doi.org/10.1002/pds.4004
- Boyce, T., & Brown, C. (2019). Economic and social impacts and benefits of health systems: report. World Health Organization Regional Office for Europe. https://iris.who.int/handle/10665/329683
- Carlson, J. (2009). Shake, don't rattle, roles. With financial pressures afoot, health systems look to change management structure. Modern Healthcare, 39(35), 6-7.
- Carman, A. L., Vanderpool, R. C., Stradtman, L. R., & Edmiston, E. A. (2019). A change-management approach to closing care gaps in a federally qualified health center: A rural Kentucky case study. Preventing Chronic Disease 16(1), 180589. https://doi.org/10.5888/pcd16.180589
- Casebeer, A., Scott, C., & Hannah, K. (2000). Transforming a health care system: Managing change for community gain. Canadian Journal of Public Health, 91(2), 89-93. https://doi.org/10.1007/bf03404917
- Chandran, L., Fleit, H. B., & Shroyer, A. L. (2013). Academic medicine change management: The power of the liaison committee on medical education accreditation process. Academic Medicine, 88(9), 1225-1231. https://doi.org/10.1097/ACM.0b013e31829e7a25
- ChePa, N., Jasin, N. M., & Bakar, N. A. A. (2017). How change management can prevent the failure of information systems implementation among Malaysian government hospitals? AIP Conference Proceedings, 1891(1), 020037. https://doi.org/10.1063/1.5005370
- ChePa, N., Jasin, N. M., & Bakar, N. A. A. (2018). Information systems implementation failure in Malaysian government hospitals: How change management helps? Journal of Telecommunication, Electronic and Computer Engineering, 10(1-11), 69-75. https://jtec.utem.edu.my/jtec/article/view/3852
- Coombe, L. L. (2008). The challenges of change management in Aboriginal community-controlled health organisations. Are there learnings for Cape York health reform? Australian Health Review, 32(4), 639-647. https://doi.org/10.1071/ah080639
- Deavin, A., Adam, S., Ausborn, S., Nielsen, A. S. B., Cappellini, S., Colmagne-Poulard, I., Gastineau, T., Gonzalez-Martinez, A., Meillerais, S., & Mortazavi, C. (2023). Path forward to optimise post-approval change management and facilitate continuous supply of medicines and vaccines of high quality worldwide. Therapeutic Innovation & Regulatory Science, 57, 7-11. https://doi.org/10.1007/s43441-022-00426-9
- Deloitte Global. (2022). Global Health Care Outlook. Are we finally seeing the long-promised transformation? https://www.deloitte.com/global/en/Industries/life-sciences-health-care/perspectives/global-health-care-sector-outlook.html
- Divaris, D., & Srigley, J. (2012). Standardized synoptic cancer pathology reporting (SCPR): Implementation strategies for population based change management initiative involving 400 pathologists across 110 hospitals. Histopathology, 99(8), 517-24.
- Enăchescu, V. A., & Trapiel, I. R. (2014). Change management in Medical University Education in Romania in the context of National and European Development Policies. Revista de Management Comparat Internaţional, 15(2), 250-255.
- Farrelly, J. S. (2022). The importance of explicit change management in health care: an example from the operating room: explicit change management in health care. Joint Commission Journal on Quality and Patient Safety, 48(1), 1-2. https://doi.org/10.1016/j.jcjq.2021.11.004
- Ferrara, L., Listorti, E., Adinolf, A., Gerardi, M. C., Ughi, N., Epis, O. M., & Tozzi, V. A. (2022). A virtuous implementation of telemedicine services in rheumatology: description of change management practices adopted by the Niguarda Hospital. Annals of the Rheumatic Diseases, 81(1), 1121. https://doi.org/10.1136/annrheumdis-2022-eular.5262
- Gibbons, J. P., Forman, S., Keogh, P., Curtin, P., Kiely, R., O'Leary, G., Skerritt, C., O'Sullivan, K., Synnott, K., Cashman, J. P., & O'Byrne, J. M. (2021). Crisis change management during COVID-19 in the elective orthopaedic hospital: Easing the trauma burden of acute hospitals. Surgeon, 19(3), e59-e66. https://doi.org/10.1016/j.surge.2020.08.008
- Godbolt, S., Williamson, J., & Wilson, A. (1997). From vision to reality - managing change in the provision of library and information services to nurses, midwives, health visitors and PAMs: (professions allied to medicine) a case study of the North Thames experience with the Inner London Consortium. Health Libraries Review, 14(2), 73-95. https://doi.org/10.1046/j.1365-2532.1997.1420073.x
- Grandpierre, A., Segler, T., & Zeiner, R. (2016). E-health - digital leadership. Pharmazeutische Industrie, 78, 939-947.
- Harris, C. C. (2023). Electronic health record modernization: VA needs to address change management challenges, user satisfaction, and system issues. GAO Reports, 1-30. https://www.gao.gov/assets/gao-23-106685.pdf
- Harrison, R., Chauhan, A., Minbashian, A., McMullan, R., & Schwarz, G. (2022). Is gaining affective commitment the missing strategy for successful change management in healthcare? Journal of Healthcare Leadership, 14, 1-4. https://doi.org/10.2147/JHL.S347987
- Harrison, R., Fischer, S., Walpola, R. L., Chauhan, A., Babalola, T., Mears, S., & Le-Dao, H. (2021). Where do models for change management, improvement and implementation meet? A systematic review of the applications of change management models in healthcare. Journal of Healthcare Leadership, 13, 85-108. https://doi.org/10.2147/JHL.S289176
- Hospodková, P., Berežná, J., Barták, M., Rogalewicz, V., Severová, L., & Svoboda, R. (2021). Change management and digital innovations in hospitals of five european countries. Healthcare (Basel), 9(11), 1508. https://doi.org/10.3390/healthcare9111508
- Hutchinson, J. (2010). Change management key to e-health. CIO. https://www.cio.com/article/208139/change-management-key-to-e-health.html
- Igoe, K. J. (2021). Change management: Why it's so important, and so challenging, in health care environments. https://www.hsph.harvard.edu/ecpe/change-management-why-its-so-important-and-so-challenging-in-health-care-environments/
- Ileri, Y. Y., & Arik, O. (2018). Investigation of resistance, perception and attitudes of employees against change in information systems using change management approach: A study in a University Hospital. Journal of Information & Knowledge Management, 17(4), 1-21. https://doi.org/10.1142/S0219649218500387
- Javanparast, S., Maddern, J., Baum, F., Freeman, T., Lawless, A., Labonté, R., & Sanders, D. (2018). Change management in an environment of ongoing primary health care system reform: A case study of Australian primary health care services. The International Journal of Health Planning and Management, 33(1), e76-e88. https://doi.org/10.1002/hpm.2413
- Jedynak, P., & Bąk, S. (2021). Risk management in crisis: Winners and losers during the COVID-19 pandemic. Routledge. https://doi.org/10.4324/9781003131366
- Karimi, E., Sohrabi, Z., & Aalaa, M. (2022). Change management in medical contexts, especially in medical education: A systematized review. Journal of Advances In Medical Education & Professionalism, 10(4), 219-227. https://doi.org/10.30476/jamp.2022.96519.1704
- Karlsson, M., & Nordström, B. (2022). Use and exchange of knowledge in the introduction of hospital-based home rehabilitation after a stroke: barriers and facilitators in change management. BMC Health Services Research, 22(1), 216. https://doi.org/10.1186/s12913-022-07618-x
- Kiernan, C., & Tunney, L. (2016). Change management within the Irish healthcare system-a doctor's conundrum. Irish Journal of Medical Science, 185, S121. https://doi.org/10.1007/s11845-015-1396-0
- Kingsley, S. (1993). Managing change in mental health services: Lessons from implementation. Journal of Mental Health, 2(4), 295-304. https://doi.org/10.3109/09638239309016964
- Kotter, J. P. (1995). Leading change: why transformation efforts fail. Harvard Business Review. https://hbr.org/1995/05/leading-change-why-transformation-efforts-fail-2
- Kulhanek, B. J. (2011). Creating effective electronic medical record change management processes. CIN: Computers, Informatics, Nursing, 29(8), 431-435. https://doi.org/10.1097/NCN.0b013e3182293726
- Law, J., McCann, D., & O'May, F. (2011). Managing change in the care of children with complex needs: Healthcare providers' perspectives. Journal of Advanced Nursing, 67(12), 2551-2560. https://doi.org/10.1111/j.1365-2648.2011.05761.x
- Lee, V., Ridzi, F., Lo, AW., & Coskun, E. (2011). A healthcare case study of team learner style and change management. Journal of Organizational Change Management, 24(6), 830-852. https://doi.org/10.1108/09534811111175788
- Levac, D., Colquhoun, H., & O'Brien, K. K. (2010). Scoping studies: advancing the methodology. Implementation Science, 5(69), 1-9. https://doi.org/10.1186/1748-5908-5-69
- Lewin's change management model (n.d.). Understanding the three stages of change. Retrieved January 19, 2024, from https://www.mindtools.com/ajm9l1e/lewins-change-management-model
- Li, H., Do, V., & Rizzuti, F. (2022). Teaching and fostering change management in medical education. Canadian Medical Education Journal, 13(3), 109-112.
- Macphee, M., & Suryaprakash, N. (2012). First-line nurse leaders' health-care change management initiatives. Journal of Nursing Management, 20(2), 249-259. https://doi.org/10.1111/j.1365-2834.2011.01338.x
- Maravi-Cardenas, A., Fuentes-Chahuaylla, M., Penafiel-Carrera, J., Mamani-Macedo, N., Raymundo-Ibanez, C., & Dominguez, F. (2020). Lean Healthcare Model using knowledge management and change management approaches to reduce delays for care in the health sector. In T. Ahram, R. Taiar, V. Gremeaux-Bader, & K. Aminian, K. (Eds.), Human Interaction, Emerging Technologies and Future Applications II. IHIET 2020. Advances in Intelligent Systems and Computing, 1152 (pp. 445-451). Springer. https://doi.org/10.1007/978-3-030-44267-5_67
- Margulies, N. (1977). Managing change in health care organizations. Medical Care, 15(8), 693-704. https://doi.org/10.1097/00005650-197708000-00010
- Martens, M., Xin Chen, H. L., & van Olmen, J. (2022). From implementation towards change management: A plea for a multi-stakeholder view on innovation implementation comment on "What managers find important for implementation of innovations in the healthcare sector - practice through six management perspectives". International Journal of Health Policy and Management, 11(12), 3118-3124 https://doi.org/10.34172/ijhpm.2022.7202
- Mazur, L. M., McCreery, J. K., & Rothenberg, L. (2010). Research and evaluation of change management initiative in rural hospitals. 60th Annual Conference and Expo of the Institute of Industrial Engineers 2010 (pp. 2698-2703).
- Munn, Z., Stern, C., Aromataris, E., Lockwood, C., & Jordan, Z. (2018). What kind of systematic review should I conduct? A proposed typology and guidance for systematic reviewers in the medical and health sciences. BMC Medical Research Methodology, 18(1), 1-7. https://doi.org/10.1186/s12874-017-0468-4
- Neuwirth, M. M., Marche, B., Kugler, C., Bures, D., Sauerland, D., Herbrandt, S., Ligges, U., Mattner, F., & Otchwemah, R. (2021). Evidence of the medical and economic benefits of implementing hygiene measures by a prevention link physician in trauma surgery: Study protocol for a biphasic multicenter prospective interventional pre-post cohort study using a structured intervention bundle development and tools of behavior change management. Contemporary Clinical Trials Communications, 23(5), 100815. https://doi.org/10.1016/j.conctc.2021.100815
- Nilsen, P., Seeing, I., Ericsson, C., Birken, S. A., & Schildmeijer, K. (2020). Characteristics of successful changes in health care organizations: an interview study with physicians, registered nurses and assistant nurses. BMC Health Services Research, 20, 147. https://doi.org/10.1186/s12913-020-4999-8
- Ningtyas, T., Larasati, E., Warsono, H., & Purnaweni, H. (2020). Describe changes management system for public organization in Indonesia (Case Study of Bureaucracy Innovation at Margono Hospital Purwokerto). Proceedings of the International Conference on Industrial Engineering and Operations Management (pp. 3839-3847). https://www.ieomsociety.org/detroit2020/papers/750.pdf
- Odaga, J., Henriksson, D. K., Nkolo, C., Tibeihaho, H., Musabe, R., Katusiime, M., Sinabulya, Z., Mucunguzi, S., Mbonye, A. K., & Valadez, J. J. (2016). Empowering districts to target priorities for improving child health service in Uganda using change management and rapid assessment methods. Global Health Action, 9(1), 30983. https://doi.org/10.3402/gha.v9.30983
- Pachamanova, D., Tilson, V., & Dwyer-Matzky, K. (2022). Machine learning, ethics, and change management: A data-driven approach to improving hospital observation unit operations. INFORMS Transactions on Education, 22(17), 178-187. https://doi.org/10.1287/ited.2021.0251ca
- Peters, M. D., Godfrey, C. M., Khalil, H., McInerney, P., Parker, D., & Soares, C. B. (2015). Guidance for conducting systematic scoping reviews. International Journal of Evidence-Based Healthcare, 13(3), 141-146. https://doi.org/10.1097/XEB.0000000000000050
- Pratt, K., Baird, G., & Gringras, P. (2012). Ensuring successful admission to hospital for young people with learning difficulties, autism and challenging behaviour: a continuous quality improvement and change management programme. Child: care, health and development, 38(6), 789-797. https://doi.org/10.1111/j.1365-2214.2011.01335.x
- Razmak, J., Bélanger, C. H., Refae, G. A. E., & Farhan, W. (2021). Electronic medical records: Taking young generations of patients and physicians through innovative technology and change management. International Journal of Electronic Healthcare, 11(3), 208-238. https://doi.org/10.1504/ijeh.2021.117121
- Ritson, N., & Waterfield, N. (2005). Managing change: the theory of constraints in the mental health service. Strategic Change, 14(8), 449-458. https://doi.org/10.1002/jsc.745
- Ruhl, S., & Klöss, T. (2012). Entwicklung medizinischer Fachabteilungen - Change Management unter Kostendruck [Development of medical specialty departments: Change management under cost pressure]. Der Klinikarzt, 41(1), 8-10. https://doi.org/10.1055/s-0032-1304524
- Sale, C., Page, D., & Penniment, M. (2019). Change management for radiation therapists - transitioning to the new Royal Adelaide Hospital. Journal of Medical Radiation Sciences, 66(3), 212-217. https://doi.org/10.1002/jmrs.345
- Saran, J. (2014). Classification and typologies as tools for pedagogical empirical research improvement. Studia i Prace Pedagogiczne, 1, 13-30.
- Saunders, M., Lewis, P., & Thornhill, A. (2009). Research methods for business students (5th ed.). Pearson Education.
- Shaban-Nejad, A., & Haarslev, V. (2007). Towards a framework for requirement change management in healthcare software applications. Proceedings of the Conference on Object-Oriented Programming Systems, Languages, and Applications (pp. 807-808). https://doi.org/10.1145/1297846.1297898
- Shipton, C., Hughes, W., & Tutt, D. (2014). Change management in practice: an ethnographic study of changes to contract requirements on a hospital project. Construction Management and Economics, 32(7-8), 787-803. https://doi.org/10.1080/01446193.2014.915336
- Shoolin, J. S. (2010). Change management - Recommendations for successful electronic medical records implementation. Applied Clinical Informatics, 1(3), 286-292. https://doi.org/10.4338/ACI-2010-01-R-0001
- Sobkowski, M., & Opala, T. (2014). Practical aspects of change management at the obstetrics and gynecology clinic at the university hospital of medical sciences in Poznań, Poland. Annals of Agricultural and Environmental Medicine, 21(2), 314-319. https://doi.org/10.5604/1232-1966.1108596
- Swecker, M., Dreon, J., Kinard, C., Ward, D., & Dougherty, C. (2010). Change management: Toy Story style. Gwinnett Health System reinvents revenue management with help from an unlikely hero. Health Management Technology, 31(3), 14-18.
- Takian, A. (2012). Envisioning electronic health record systems as change management: the experience of an English hospital joining the National Programme for Information Technology. Studies in Health Technology and Informatics, 180, 901-905. https://doi.org/10.3233/978-1-61499-101-4-901
- Thistlethwaite, J. E. (2000). Introducing community-based teaching of third year medical students: Outcomes of a pilot project one year later and implications for managing change. Education for Health, 13(1), 53-62. https://doi.org/10.1080/135762800110574
- Threatt, T., Pirtle, C. J., Dzwonkowski, J., & Johnson, K. B. (2020). Using a custom mobile application for change management in an electronic health record implementation. JAMIA Open, 3(1), 37-43. https://doi.org/10.1093/JAMIAOPEN/OOZ048
- Torkzadeh, J., & Mohtaram, M. (2022). Developing a framework for managing change climate in social systems: Some practical implications for medical education universities. Education Research International, 3, 1-9. https://doi.org/10.1155/2022/9352882
- Turja, T. (2022). Rather sooner than later: Participatory change management associated with greater job satisfaction in healthcare. Journal of Advanced Nursing, 78(3), e49-e51. https://doi.org/10.1111/jan.15133
- van Rossum, L., Aij, K. H., Simons, F. E., van der Eng, N., & ten Have, W. D. (2016). Lean healthcare from a change management perspective: The role of leadership and workforce flexibility in an operating theatre. Journal of Health Organization and Management, 30(3), 475-493. https://doi.org/10.1108/JHOM-06-2014-0090
- Vickers, S. M., Agarwal, A., Patel, N., Benveniste, E. N., Bulgarella, D., Fouad, M. N., Hoesley, C., Jones, K., Kimberly, R. P., Rogers, D. A., Larson, J. A., Leeth, T. R., Mack, L., Dorman, P., Furgerson, T., Longshore, J., & Watts, R. L. (2021). Returning to growth: One Academic Medical Center's successful five-step approach to change management. Academic Medicine: Journal of the Association of American Medical Colleges, 96(10), 1401-1407. https://doi.org/10.1097/ACM.0000000000004116
- Villalbí, J. R., & Farrés, J. (2005). Culminar la reforma de la atención primaria de salud: gestión del cambio en Barcelona, 1998-2003 [Rounding off the reform of primary health care: Managing change in Barcelona, 1998-2003]. Atencion Primaria, 35(9), 484-488. https://doi.org/10.1157/13075474
- Walsh, K. (2016). Cost and value in medical education: The factor of change management. The Pan African Medical Journal, 24, 246. https://doi.org/10.11604/pamj.2016.24.246.6841
- Ward, R. A., Ting, A. S. J., & Peyton, E. M. (2020). A medical student's perspective on "students as catalysts for curricular innovation: A change management framework." Medical Teacher, 42(12), 1427-1428. https://doi.org/10.1080/0142159X.2020.1739256
- Webster, R. J. (2023). Climate action, staff engagement, and change management: A pediatric hospital case study. Healthcare Management Forum, 36(4), 195-198. https://doi.org/10.1177/08404704231165482
- Yousefi, M., Mashhadi, L., Akbarisari, A., & Ebrahimi, Z. (2022). Change management in hospitals: A framework analysis. Studies in Health Technology and Informatics, 299, 262-268. https://doi.org/10.3233/SHTI220995
- Yusif, S., Hafeez-Baig, A., & Soar, J. (2022). Change management and adoption of health information technology (HIT)/eHealth in public hospitals in Ghana: A qualitative study. Applied Computing and Informatics, 18, 279-289. https://doi.org/10.1016/j.aci.2019.11.007







 https://orcid.org/0000-0001-5025-1607
https://orcid.org/0000-0001-5025-1607